
Exponential Medicine — Artificial Intelligence + Robotic Surgery
Upcoming developments of artificial intelligence (AI) combined with robotic assisted surgery (RAS) will lead to dedicated systems, reduced cost + complexity and with the higher precision to increased clinical acceptance.
ABSTRACT
Healthcare will experience a lot of changes in the next 10 years. Intentional technology based disruptions will have an effect on the actual delivery, but also come with novel health business models. The article will initially present some of the upcoming developments and subsequently focus the discussion on artificial intelligence (AI) and robotic assisted surgery. The combination of these technologies will lead to dedicated systems, reduced cost and complexity and with higher precision to increased aceptance. Future developments and the education of technical and clinical disciplines however needs to be more aligned and be conducted in interdisciplinary setups.
KEYWORDS
artificial intelligence (AI), interdisciplinarity, exponential medicine, Robotic Assisted Surgery (RAS)
INTRODUCTION
Healthcare is in a state of upheaval globally, but in some cases does not yet know it or does not want to admit it. Technological developments, especially the so-called exponential technologies, are one of the main reasons. Exponential technologies are digitally based approaches that challenge current methods / practices and usually overtake and replace them faster than expected (disruption).
Why shouldn't healthcare change dramatically with the advent of these digitally based and exponentially improving technologies? In most healthcare systems, the diagnosis and subsequent therapy of a disease state is rewarded. A healthy person is not a patient and therefore not (yet) really interesting for value creation in the health business model.
Innovations in the field of health are currently always scrutinized for their business viability, which is often difficult to demonstrate at the moment, especially in the case of preventive care issues. And actually, we have enough doctors, enough hospitals, enough technology, everything is always getting a little (incrementally) better, and we also have enough money. Really? What about increasing life expectancy, changing demographics, ever-increasing costs, ever-increasing demand for caregivers, and perhaps the future problems of new viruses and their impact on the system.
If we look at other health care systems, for example in India and Africa, we will also see other problems. Unequal access to health care depending on socio-economic conditions, unequal distribution of care facilities in rural versus urban structures, few well-trained specialists and diagnosis / therapy is very expensive relative to income. These are problems that we do not have in the developed world, but which will lead to new health approaches in the global innovation environment in these countries, which will then also have a direct influence on our care and our business models in the medium term [1].
In this respect, we can safely assume that artificial intelligence / machine learning in all medical fields, robotics in surgery, augmented and virtual reality (AR / VR) in diagnosis and therapy, genetics in all fields, 3D printing of tissue and bone, and advances in imaging and sensor technology will significantly change healthcare in the future - and probably much faster than expected.
Future health innovations will be guided by the 4P's. Health needs to be PREVENTIVE and PREDICTIVE to be able to treat a developing disease as early as possible, must of course be PERSONALISED (also known as PRECISION MEDICINE) to the individual and let people PARTICIPATE in their own health development.
And a 5th ‘P’ should be added for PROLONGED HEALTH, a definite goal of future health innovation design, or in other words an increased lifespan with an equally increased healthspan.
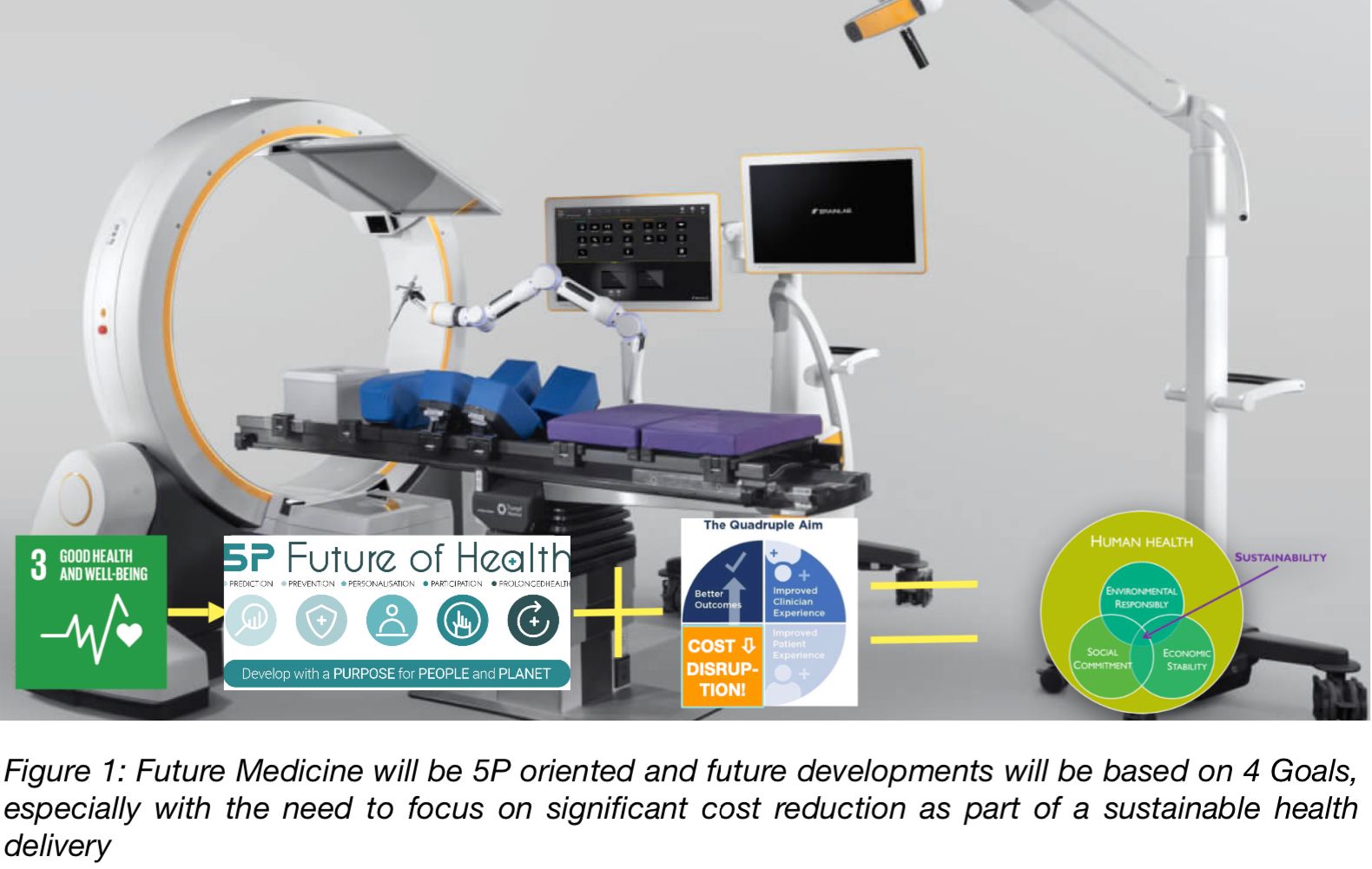
In addition, the developments of new systems / products and processes should have the following objectives:
1. improve clinical outcomes,
2. and 3. improve the clinical environment and health system experience for patients and clinical staff, and
4. significantly reduce the cost of systems and processes.
Only with such cost reductions can disruptive solutions be developed to solve the global problems mentioned earlier (see Figure 1.).
But honestly, at the moment we are mainly researching and developing incrementally - making small advances and thus increasing costs disproportionately. We all know, of course, that sustainable health depends only to a small extent on the quality of health care and to a much greater extent on individual lifestyles, quality and quantity of nutrition, as well as the economic environment and an intact living environment.
Should we be able to detect diseases at a very early stage in the short and medium term - e.g., through sensor technology, artificial intelligence at home and connection with gene analyses and corresponding evaluations - and thus avoid a severe course of disease, then that would certainly be in the interest of everyone.
But what does that mean for the number of hospital beds or for inpatient care in general? How will this be rewarded? What function will physicians assume in the future? What will the business model HEALTH look like?
The introduction should sensitize the reader somewhat on the needed developments and health delivery changes and also to point out once again that we are usually significantly overestimating the speed of technological implementation and that is especially valid for any innovations in healthcare that challenge the current setup.
Many of the things that futurologists are citing at the moment are not really reasonably applicable or are far too big and far too expensive and thus, in the mind of the beholder, very far away in terms of time for implementation in the health segment mainly due to the reluctance of the current stakeholders. But this can change very fast and we have already misjudged developments often!
In the following I would like to become a little more concrete and actually only describe robotics and artificial intelligence (here together with all other technologies of machine learning). In doing so, I will also discuss the current advantages and disadvantages, and I will list the next development steps, in order to be able to give a basis for an outlook at the end.
Figure 1 shows an example of a modern surgical workstation with imaging, navigation, robotics and corresponding analysis software (Brainlab, Munich).
However, please think now for a moment about what could change for you in the future and how an adapted training and innovation generation could look like. No one knows how the future will actually unfold, but a plan and imagination can at least be adapted.
"Any sufficiently advanced technology is indistinguishable from magic", third law of Sir Arthur Clarke (futurist, author, inventor) from 1973 fits quite well in this context!
SURGERY 3.0 / 4.0
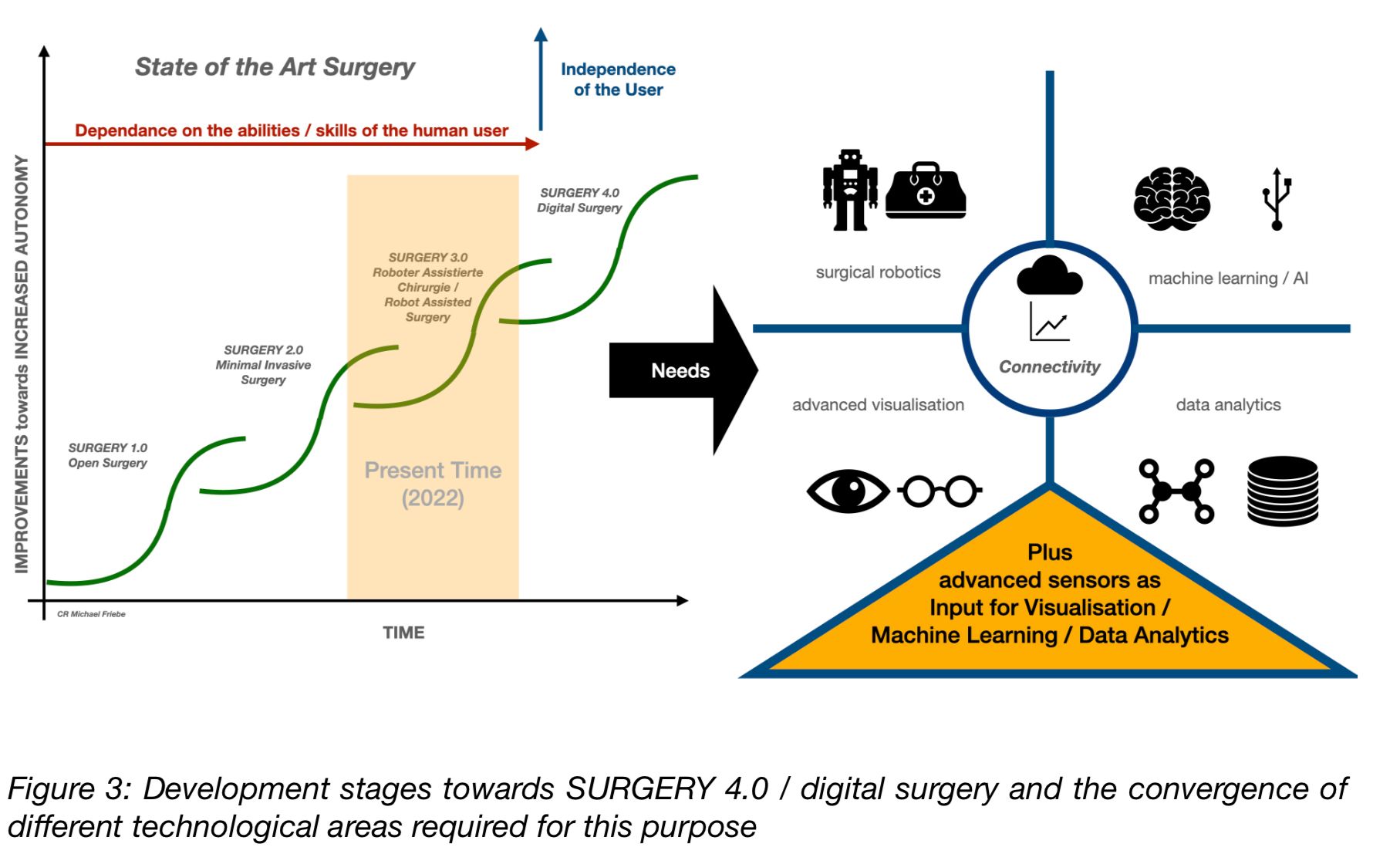
Open surgery (SURGERY 1.0) has been significantly improved for the patient in many areas in recent decades through the use of keyhole technologies / minimally invasive surgery (SURGERY 2.0). Since 1995 there are now Robotic Assisted Surgery (RAS) or the evolution to SURGERY 3.0 (see Figure 2).
However, there is a rather sobering record of robotic-assisted surgery. The studies published so far and analyzed below have shown that it actually makes no difference so far whether patients are operated on with or without robotics. The presence of a surgical robot was not decisive for success, but the experience of the surgeon.
The surgeon bears a very great responsibility towards the patient. The smallest intervention on the patient's body can make the difference between irreparable damage and unexpected recovery. New digital technologies will expand the surgeon's capabilities and improve the chances of success and will not replace him in the medium term. However, patient empathy before and after the surgical procedure would definitely secure the position and value of the clinician in the long term. Currently, this is however not always a proven strength of surgeons [2].
The nucleus (… and cash cow) of a hospital is surgery. On the one hand, the operating room is a profit center, but on the other hand, it is often the place with the lowest efficiency. In order to deliver better and consistently good quality of care for every patient, machine learning / artificial intelligence should be used, and the knowledge gained about "best practices" should be made globally available. For this, however, we need a fully digitized surgery [3].
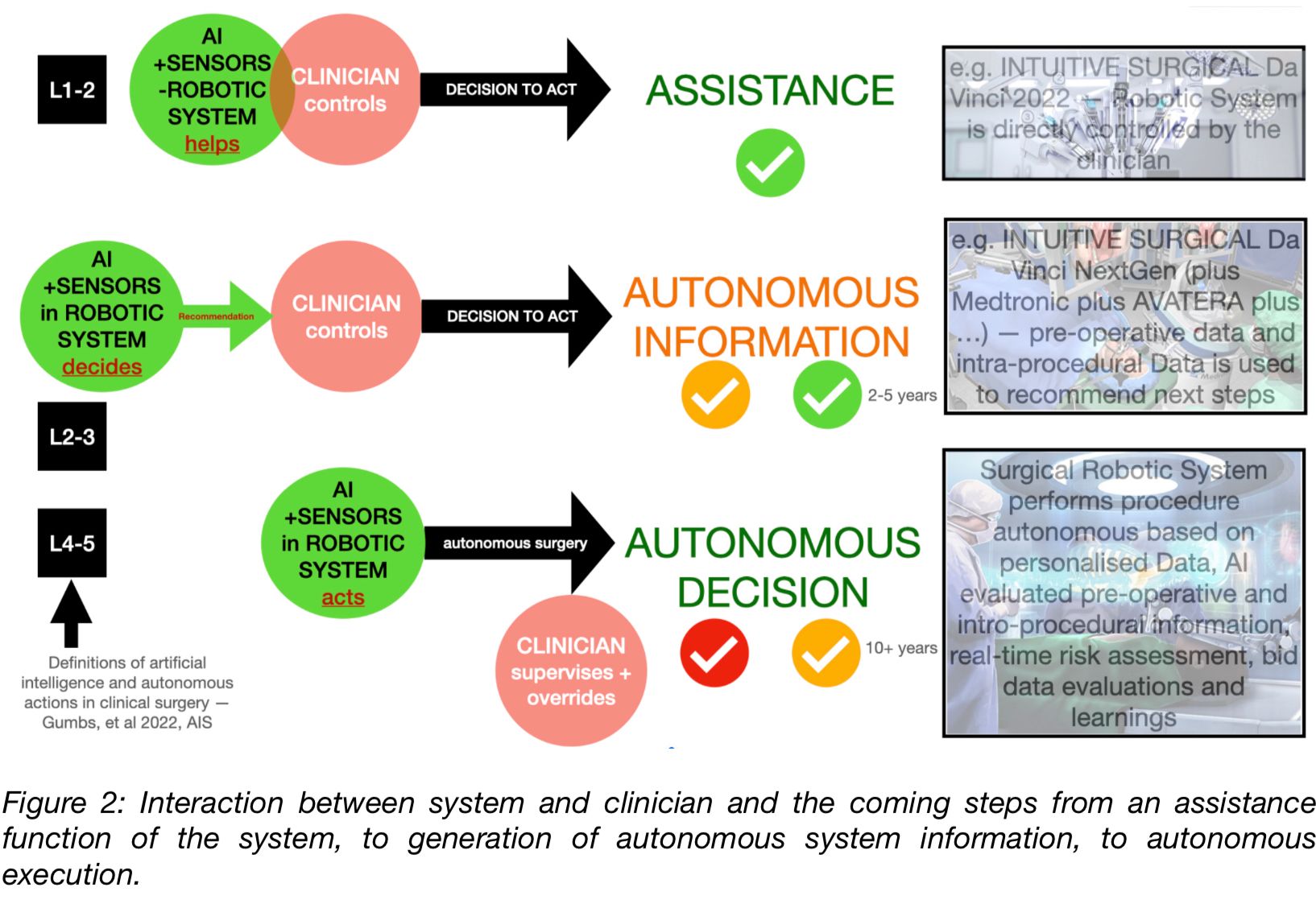
Another breakthrough will certainly come with the introduction of more or less autonomous robotic systems. Although it will certainly take some time until then, these systems will get their place. First, the developments of digital surgery (SURGERY 4.0) in the combination of improved visualization (optical, integration of other diagnostic systems, image processing, and display), as well as globally networked data analysis in advance (patient individualized) of a procedure and the integration of artificial intelligence will once again significantly expand the quality and the possible applications. The dependence on the clinical user's ability will also be significantly reduced due to the higher level of computer-generated support and automation that will then be available and the lower learning effort required (for more on this, see Figure 3). [4]
STATUS QUO ROBOTIC + ARTIFICIAL INTELLIGENCE IN SURGERY
Most of the nearly 10,000 RAS systems currently installed globally (60% USA, 20% Europe, nearly 80% market share by INTUITIVE SURGICAL) are merely assistance systems directly controlled by the clinician / surgeon. New device sales amounted to € 4.5 billion in 2020 with an expected increase in sales to almost € 15 billion in 2030 with an anticipated 40,000 installed systems, which will then also be able to provide autonomous decisions and, in certain areas also already autonomously decide or perform a surgical operation independently under the responsibility of a clinician [5].
Robotics in surgery, although not yet clearly clinically advantageous, is undoubtedly already highly significant for attractiveness and external marketing towards potential patients. Because of the higher precision, there is a reduction in surgical and post-operative complications when using robotics. Due to the relaxed and less stressful position, there is also less physical strain for the surgeon performing the procedure. However, this is currently offset by the high cost of training, a rather low utilization, and very high capital and operational costs. The technical complexity of the systems is very high due to the many different fields of application, and the preparation time is, therefore correspondingly long. In the meantime, there are almost 20 companies offering commercial products, and a large number of start-ups are trying to establish themselves in this segment. It is foreseeable that there will be more specialized, smaller, and less complex systems in the very near future, which will then likely also be significantly cheaper to purchase and maintain. All will be equipped with more and more artificial intelligence, provide autonomous information, and solve the current disadvantages in the medium term (see Figure 4.).
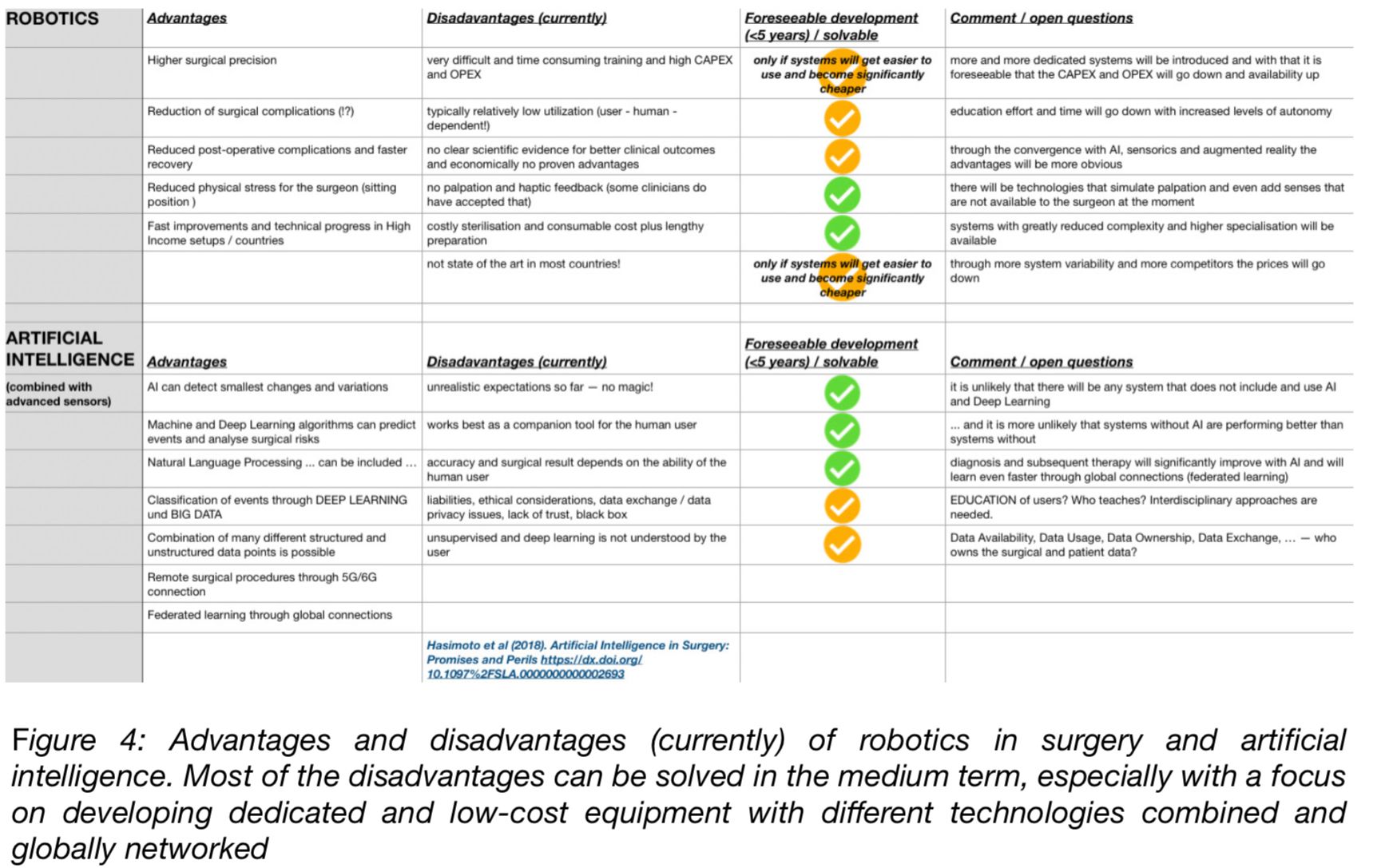
The advantages of networked data exchange for improving artificial intelligence are obvious. Digitally recorded experience can be used globally to improve the systems. For this to happen, improved data security and standardization of data formats are required. Artificial intelligence is able to combine many structured and unstructured data points and use them, for example, to make predictions about certain interventions or to detect even the smallest changes at an early stage during the intervention. Of course, there are still too few data points and too few case studies to reliably use them for autonomous surgical decision-making.
SUMMARY AND OUTLOOK
Complex technical systems without artificial intelligence will probably no longer exist in the future. Very fast networked "learning" these systems will be able to prove their advantages in future studies. In this respect, we can pretty safely assume that robotics in surgery combined with artificial intelligence, deep and federated learning, and 5G or 6G technology will shape the future.
While we talk about SURGERY 4.0 or INDUSTRY 4.0, we are still educating the users at a perceived level 2.5. We do not teach future foresight in innovation generation, are ignorant of likely changes in business models, and educate in siloed structures. The engineer has little - and if any - intensive contact with clinical staff, and clinical disciplines often have little or no input toward the development of new systems and approaches. There needs to be an EDUCATION 4.0, which is much more interdisciplinary and teaches the clinician the technical basics, and on the other hand, teaches the engineer how to work clinically and teaches everyone more empathy and future innovation methodology [6, 7].
Surgeons are in a key position in the introduction of artificial intelligence in the clinical setting. AI could revolutionize education and significantly improve the quality of patient care in the future. The clinical environment, and surgery in particular, will need to work closely with data scientists in the future to achieve this [8, 9]. Innovation will be interdisciplinary, and for this to happen, there needs to be much more cross-disciplinary research and development. Innovation is actually only innovation when it reaches the patient and generates significant added value, which is very often generated by a significant reduction in treatment costs.
In the future, we will record digital data in all areas of healthcare, link them together, and then be able to make risk predictions and plan and implement the appropriate interventions. This will then open up completely new business models and healthcare will then also revolve more around the health of the patient.
REFERENCES
[1] Friebe M (2020). Healthcare in need of innovation: exponential technology and biomedical entrepreneurship as solution providers (Keynote Paper). Proc. SPIE 11315, Medical Imaging 2020: Image-Guided Procedures, Robotic Interventions, and Modeling, 113150T https://doi.org/10.1117/12.2556776
[2] Zylka-Menhorn V (2019). Roboterassistierte Chirurgie: Kostenintensiv – bei eher dünner Evidenzlage. Dtsch Arztebl 2019; 116(26): A-1278 / B-1053 / C-1041 (https://www.aerzteblatt.de/archiv/208505/Roboterassistierte-Chirurgie-Kostenintensiv-bei-eher-duenner-Evidenzlage)
[3] Vilsmeier S (2021). Leveraging AI and Digital Technologies for Healthcare in 2021 and beyond. https://www.brainlab.com/de/journal/leveraging-ai-and-digital-technologies-for-healthcare/
[4] Mesko B (2021). The Technological Future Of Surgery. https://medicalfuturist.com/the-technological-future-of-surgery/
[5] Nakanishi T, Lee S-H (2021). Global Surgical Robots Market. BIS Research. https://bisresearch.com/industry-report/global-surgical-robotics-market-2025.html
[6] O’Sullivan S, …, Friebe M, et al. (2019). Operational framework and training standard requirements for AI-empowered robotic surgery. The International Journal of Medical Robotics and Computer Assisted Surgery V0l 16, Issue 5, pages 1-13, https://doi.org/10.1002/rcs.2020
[7] Friebe M (2020). HealthTEC Innovation Design - a proposal for a novel Master degree program based on Unmet Clinical Need, global Healthcare Challenges, and 21st-century skills. Current Directions in Biomedical Engineering 2020; 6(3): 20203153. https://doi.org/10.1515/cdbme-2020-3153
[8] Hasimoto et al (2018). Artificial Intelligence in Surgery: Promises and Perils https://dx.doi.org/10.1097%2FSLA.0000000000002693
[9] Smith R (2019). How Robots and AI are Creating the 21st-Century Surgeon. https://www.roboticsbusinessreview.com/health-medical/how-robots-and-ai-are-creating-the-21st-century-surgeon/

About the Author
Serial entrepreneur in the field of medical technology, inventor and developer (over 100 patent applications), and health innovation researcher. After studying electrical engineering, he worked for five years as a development engineer in the Bay Area (magnetic resonance tomography) and, in parallel, earned a business degree. After returning to Germany, he obtained a Ph.D. with a topic on interventional magnetic resonance imaging and subsequently founded the first company in the German Ruhr area. From 2015-2019 he was the chair of the technical faculty of Otto von Guericke University in Magdeburg, and since 2020 he has been an honorary professor at the medical faculty. Since 2022 he is also a guest research professor at the AGH University of Krakow and the founding director of the CIBE - Center for Innovation, Business Development, and Entrepreneurship at the FOM University of Applied Sciences in Essen, Germany.
ExO Insight Newsletter
Join the newsletter to receive the latest updates in your inbox.









