Declining American Life Expectancy And What to Do About It
The United States faces a critical choice: accept a decline in life expectancy or enhance the nation's vibrancy through innovation and connectedness, inspired by the vitality of the world's Blue Zones.
Longevity paired with vitality - this is the blueprint offered by the world's Blue Zones. Yet America lags behind, with declining life expectancy and quality. We face a choice: accept this fate, or amplify our nation's vibrancy through innovation and connectedness.
Introduction
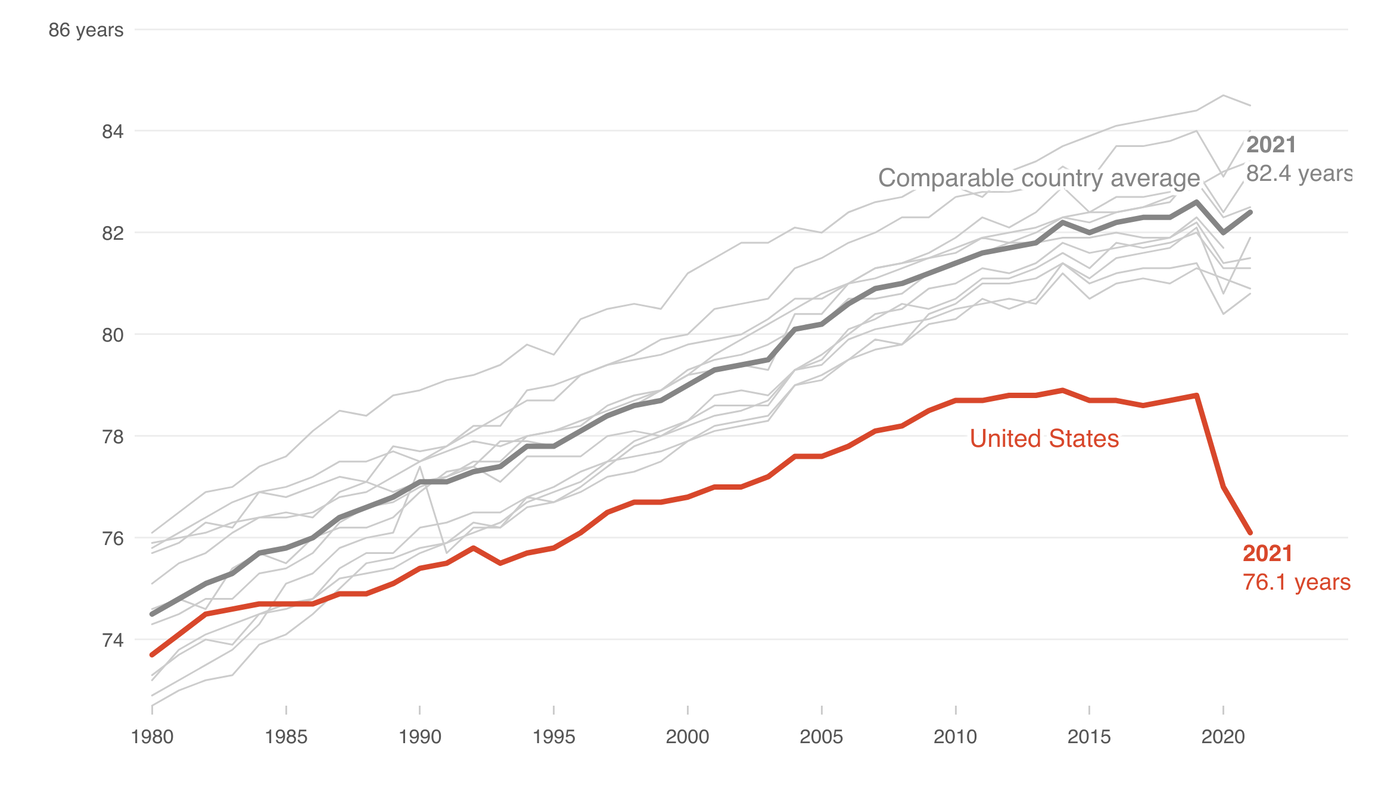
In today's world, where medical advancements are at their peak, it's alarming to witness a decline in life expectancy in the United States. The recent data from the Centers for Disease Control and Prevention (CDC) indicates a drop to 76.4 years, a figure not seen in almost two decades. However, there are regions in the world, known as the Blue Zones, where longevity is paired with remarkable life quality. The Netflix series "Live to 100: Secrets of the Blue Zones" provides a deep dive into these regions. Dan Buettner, an explorer and best-selling author, showcases places like Okinawa, Japan; Sardinia, and California, where living past 100 is common. But what's more impressive is the quality of life these centenarians enjoy.
In Blue Zones, individuals don't just live longer; they live better. Their cognitive functions remain sharp, and they continue to be active both socially and physically. They enjoy a health span, not just a lifespan. This means that they spend a significant portion of their lives free from chronic diseases and disabilities. For instance, in Okinawa, it's common to see elderly individuals participating in community activities, practicing traditional dances, or even working in their gardens. Their diets, rich in vegetables and low in processed foods, coupled with regular physical activity, contribute to their robust health. Social connections, a sense of purpose, and community involvement further enhance their well-being.
This stark contrast between the declining life expectancy in the US and the thriving health span in Blue Zones raises a pressing question: What factors contribute to such a disparity, and how can the US learn from these regions to improve both longevity and life quality?
The Causes
The decline in American life expectancy is a multifaceted issue, with several intertwining causes:
Opioid Crisis: According to the National Institute on Drug Abuse, in 2019 alone, there were 49,860 reported opioid-related deaths in the U.S. This epidemic, driven by both prescription and non-prescription opioid drugs, has significantly impacted life expectancy.
Mental Health: The CDC reports that suicide rates have increased by 33% from 1999 to 2019. Mental health disorders, often undiagnosed or untreated, have become a silent epidemic, further driving down life expectancy.
Economic Disparities: A study published in JAMA found that individuals in the wealthiest 1% live 10 to 15 years longer than those in the poorest 1%. Access to healthcare, quality of life, and exposure to environmental hazards vary dramatically across economic strata, leading to disparate health outcomes.
Lifestyle Diseases: Sedentary lifestyles and poor dietary habits have led to a surge in diseases like obesity, diabetes, and heart disease. The CDC states that heart disease remains the leading cause of death in the U.S., with over 696,000 deaths in 2020.
Access to Healthcare: Despite being one of the wealthiest nations, many Americans lack access to basic healthcare. The Census Bureau reported that in 2019, 26.1 million Americans did not have health insurance at any point during the year.
To truly understand and address the decline in life expectancy, it's crucial to recognize these causes and the intricate ways they intersect and impact the health of the nation.
The Power of Empathetic Design Thinking
At the heart of transformative healthcare solutions lies empathetic design thinking. It's about delving deep into the lives of patients, understanding their unique challenges, and crafting solutions that resonate. Ethnographic research offers a window into patients' worlds, revealing nuances often overlooked. For instance, something as simple as providing transportation can make a world of difference for low-mobility patients.
However, beyond the physical needs, there's a profound importance in addressing emotional and social well-being. The Okinawan concept of "moai" serves as a testament to the power of social connections. In Okinawa, "moai" refers to groups of friends who come together for mutual support. They meet regularly, share life experiences, offer advice, and even provide financial assistance when needed. This deep-rooted sense of community and belonging has been linked to reduced stress, increased happiness, and longer life.
Incorporating such community-driven support systems can be transformative. Imagine healthcare solutions that don't just treat diseases but also foster community connections, ensuring that individuals feel supported, valued, and understood. By placing patients at the core of solution design and integrating holistic well-being approaches like the "moai", we can ensure that interventions are not just effective but also empathetic.
Leveraging Exponential Technologies
The digital revolution offers a beacon of hope for healthcare. Telehealth platforms are democratizing access, ensuring that quality care isn't bound by geographical constraints. Advanced data analytics tools are decoding complex health patterns, paving the way for personalized interventions. Collaborative ecosystems, where healthcare organizations join forces, can accelerate the prototyping and deployment of groundbreaking solutions.
Building on this, the ExO model, which emphasizes leveraging community and social attributes, can be a game-changer for elderly care. For instance:
Community & Crowd: By tapping into the collective intelligence and resources of a community, healthcare organizations can co-create solutions tailored for the elderly. Platforms that connect elderly individuals with volunteers or professionals for companionship, assistance, or skill-sharing can foster a sense of belonging and purpose.
Social: Harnessing the power of social networks can help in disseminating health information, connecting the elderly with support groups, and even facilitating virtual community events. Moreover, platforms that allow the elderly to share their life experiences, wisdom, and stories can make them feel valued and needed.
By integrating the ExO attributes into healthcare solutions, we can create systems where the elderly don't just receive medical care but also experience social and emotional support. This holistic approach, which combines technology with community-driven initiatives, holds the promise of enhancing both the quality and longevity of life.
Policy Reforms: The Need for Innovation
While technological advancements and community-driven initiatives are crucial, they can only go so far without the backing of robust policy reforms. The traditional approach to policy-making, characterized by its slow pace and bureaucratic hurdles, is ill-suited for the rapidly evolving challenges of today's healthcare landscape.
One of the primary issues is the inertia in government agencies. While stability and caution are essential in governance, there's a pressing need for these agencies to adopt a more experimental mindset. This doesn't mean recklessly implementing untested policies but rather fostering an environment where innovative ideas can be piloted, assessed, and scaled.
Several grant programs, like those from the NHS and NSF, hint at this shift towards innovation. However, the awareness and accessibility of these grants remain limited. Moreover, while research is vital, an overemphasis on it can stifle the iterative development and deployment of solutions. Programs like the NSF POSE Phase II grant are commendable examples of this balance, but they are exceptions rather than the norm.
Some potential ways policymakers could truly drive change:
XPRIZE Style Competitions: Governments can sponsor competitions that challenge innovators to address specific healthcare issues. These competitions, combined with grant funding, can catalyze groundbreaking solutions.
Mastering Media: Government agencies need to leverage media effectively to raise awareness about grants, competitions, and other initiatives. A well-informed public can be the best ally in driving healthcare innovation.
Iterative Development: Instead of solely focusing on research, there should be a shift towards iterative development. This means piloting solutions, gathering feedback, making improvements, and then deploying them at scale.
In essence, for America to reclaim its vitality and reverse the declining life expectancy trend, policymakers must not only prioritize health but also be willing to innovate in their approach to governance.
What Now?
The path forward is clear - we must foster a societal movement that prioritizes holistic wellbeing. Technology can help connect us, but we must strengthen our human bonds. Policy can enable change, but we must demand innovation. Medical advances can cure illness, but we must champion prevention. The Blue Zones shine as examples, but we must blaze our own trail.
True transformation starts with everyday conversations - between parents and children, friends and neighbors, communities and leaders. We each hold a piece of the puzzle, a thread in the tapestry of change. It is by weaving together our diverse perspectives that we can craft solutions that uplift us all.
We stand at a pivotal moment, a crossroads between declining and thriving. The choice is ours. Will we succumb to disillusionment? Or will we rise up to reignite our nation's vibrancy? The potential lies within us, within each conversation, idea, and act of compassion. But potential alone is not enough. We must act. We must engage.
The time for change is right now. Waiting is just another day of dying instead of living.
#LifeExpectancy #BlueZones #HealthcareInnovation #Longevity #Wellbeing #EmpatheticDesign #CommunitySupport #TechnologyInHealthcare #PolicyReforms #QualityOfLife #HolisticWellness #VibrantNation #HealthcareSolutions #SocialConnectedness #ChooseChange
Sources:


Participate in the weekly ExO Masterminds sessions by Registering here
Immerse yourself in the game-changing ideas of OpenExO.
Begin your journey here 🎟️ExOPass & 📚Exponential Organizations 2.0
ExO Insight Newsletter
Join the newsletter to receive the latest updates in your inbox.